Shoeing for Palmar Hoof Pain |
|||||||||||||||||||||||||||||||||||||||||||||
Introduction
|
|||||||||||||||||||||||||||||||||||||||||||||
Palmar hoof pain (PHP) is usually defined as a positive reaction (absence or decrease of lameness) after a distal palmar digital nerve block ( DPDN block near the margin of the ungular cartilages). Although sometimes defined as a “heel block”, it anesthetizes the DIP joint, the entire sole, the distal phalanx (PIII) and the navicular apparatus ( 1/ Schumacher 2006) Besides podotrocleosis, which in itself is a condition which encompasses more than just “naviculitis “or “navicular syndrome “, PHP may therefore be due to: |
|||||||||||||||||||||||||||||||||||||||||||||
Clinical examination |
|||||||||||||||||||||||||||||||||||||||||||||
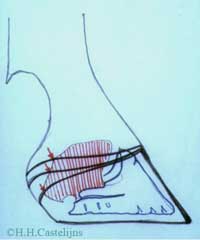
Careful clinical examination, including inspection, palpation, pulse taking and judicious use of hoof testers ( before anesthesia of course ), remains the most valuable tool in differentiating among the different conditions mentioned above. This examination requires patience and more clinical skills than is often assumed, but can , together with a good history work up, often save a lot of frustration . An especially valuable clinical test is the digital extension / elevation test. Traditionally done with a board, this test evaluates the horse’s tolerance to dorsal extension, ( 2/Desbrosse, 2002).[ fig.1.a,b,c,]. |
|||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||
A graduated Digital Extension Device ( DED) has been developed by the author which , besides measuring the exact degrees of tolerance to the dorsal extension of each forelimb, also permits evaluation and measurement of the tolerance to lateral and medial elevation of the foot, which causes collateromotion of the DIP joint ( 3/ Chateau et al, 2002). Tolerance to dorsal extension is variable for each limb, depending on conformation, and can vary in sound horses from around 30° ( some quarter horses with straight short pasterns and “ tighter “ deep digital flexor tendons (DDFTs), to over 45° ( e.g. some thorough bred horses with long oblique pasterns ,and lax DDFTs). Sound horses tolerate lateral and medial elevations of the foot till the opposite side of the foot lifts off the surface of the DED. The degree of elevation at which this occurs , is much more standardized across breed- and conformation types, than dorsal elevation; typically being 19° of lateral elevation and 20-21° of medial elevation. Differences between lateral and medial degrees, are probably due to the fact that the test isperformed with the opposite limb held off the ground, whereby the horse places the weight bearing , and tested , limb , closer to the midline of its body. Intolerance to dorsal extension may indicate : Intolerance to lateral or medial elevation may indicate: Finally, there are conditions which might reduce tolerance to extension in a combination of directions: dorsal and lateral, dorsal and medial, lateral and medial, all three. |
|||||||||||||||||||||||||||||||||||||||||||||
Diagnostic Imaging |
|||||||||||||||||||||||||||||||||||||||||||||
In recent years diagnostic imaging has made great strides, as first ultrasound and then MRI and CAT have allowed for much more detail when “looking” into the foot. High quality, ( digital) X rays, including the use of contrast material, have also progressed, but the great difference is certainly the ability to better detect soft tissue injuries, which generally precede bony lesions.[ fig.2] |
|||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||
Better diagnostics though, also means finding more lesions, often in different , even adjacent structures, each of which theoretically requires different biomechanical solutions ( read shoeing strategies ) . This is another point which indicates the importance of a good, clinical work up; e.g. if a lesion in the distal DDFT, adjacent to a lesion in the straight distal sesamoidean ligament is detected, it is necessary to find out if the horse resents dorsal digital extension more than fetlock extension, before prescribing therapeutic shoeing. [ fig.3.a,b.]. |
|||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||
Therapeutic shoeing techniques |
|||||||||||||||||||||||||||||||||||||||||||||
The following elements should be taken into account when considering shoeing prescriptions: The last element is of paramount importance, because a lot of shoeing techniques which are based on changing around the ground wearing surface of the shoe, only work on penetrable ground. As far as the type of work goes, some disciplines require an enormous amount of work on ( tight) circles others do not ( e.g. standard bred racing). Some lesions hold out hope for eventual healing ( e.g. some soft tissue injuries ), and the therapeutic shoeing will only be temporary; other lesions are permanent ( e.g. ring bone),and therapeutic shoeing techniques will be necessary for the rest of the horse’s (working) life. General objectives of therapeutic shoeing is to spare painful structures, but this can only be done by loading other structures more: e.g.: a reverse shoe on soft ground relieves the DDFT, but loads the superficial DFT and the suspensory ligament ( S:L.) more. |
|||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||
Discussion: |
|||||||||||||||||||||||||||||||||||||||||||||
Table 2 shows the importance of basing the different shoeing techniques on digital extension test results; it is hard to make a horse worse, when using this as a guideline. Immediate ( lack of) results can be deceiving; shoeing can be described as a 10-15 minute flexion test ( per limb), with percussion. Specially in the case of chronic pathologies , a horse should be allowed 15 to 20 days to show improvement, before concluding that the shoeing is not helping ( enough). During this period it is preferable not to change medication if one wants to judge the incidence of the shoeing changes. Management advice, and owners’ compliance with this advice, can be as important as many other treatments, including therapeutic shoeing; e.g. a horse with chronic DIP artrosis does not enjoy lounging on a tight circle , while daily turnout can be positive. Compact versus penetrable ( deep) ground is important in the shoeing decisions as some techniques like bar shoes or wide webs to one side only work on penetrable ground. Ease of all around break over ( not only dorsal ) is key on compact ground. Naturally, there is a whole range of conditions which lay between compact and deep; modern arenas for example , often have a lot of elasticity, but not as much penetration as older, deeper ones. Notably absent from table 2,are shoeing techniques with raised heel shoes or heel wedges. The principle behind raised heel shoeing is that if flexes the DIP joint. Most heel wedges and raised heel shoes have a 2-3° wedge. A recent study showed that part of the heel raise is taken up by vertical- proximal deformation of the hoof capsule at the heels.[fig.16,a,b.] ( 6/Castelijns). Also, heels tend to grow less and wear more with these methods, often ending up at the status quo ante ( and worse quality heels), as far as the DIP joint mechanics in the sagittal plane goes. |
|||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||
If ( temporary) heel raises are to be attempted in horses with intolerance to dorsal extension, it is certainly preferable to use frog and sole support systems, like for instance the PM. hoof pads and condensation silicone combination, or the MyronMcLane pad. [fig.17]. These systems have the added advantage that they will limit heel penetration in deep ground ( which is a form of hyperextension of the DIP joint). |
|||||||||||||||||||||||||||||||||||||||||||||
|
|||||||||||||||||||||||||||||||||||||||||||||
Finally, it is the author’s hope that equine podiatry will move beyond the fixed shoeing prescriptions for general conditions. As diagnostic procedures have improved and become more specific and precise, so should therapeutic shoeing |
|||||||||||||||||||||||||||||||||||||||||||||
References: |
|||||||||||||||||||||||||||||||||||||||||||||
1 Schumacher, J.; Anesthesia of the foot, proceedings XII SIVE congress, 28-29-/01/2006, p.56-58. 2 Desbrosse, F. ; L’exploration physique du pied. Inspection, palpation, pression et mobilisation articulaire. Pratique vétérinaire Equine, Vol. 43, p. 17-27, 2002. 3 Château, H. Degeurce, C- Denoix, J.M ; Biomécanique du pied du cheval. Pratique Vétérinaire Equine, Vol. 34, p. 7-15, 2002. 4 Castelijns, H.H ; L'uso di un apparecchio di estensione digitale graduato nella diagnosi di zoppia.XII Congresso Multisala SIVE - Bologna - Italia 27-29/01/2006 5 Leveillard,D: personal comunication, 2005 6 Castelijns, H.H.; Pathogenesis and treatment of spontaneous quarter cracks quantifying vertical mobility of the hoof capsule at the heels. Pferdeheilhunde , Volume 5 /2006, p. 569-576. Note: The author gets none of his income from the sale of any of the commercial products mentioned in this article included the DED |
|||||||||||||||||||||||||||||||||||||||||||||